Participatory co-design to improve the monitoring of users in the ER
by: Vera Oliveira
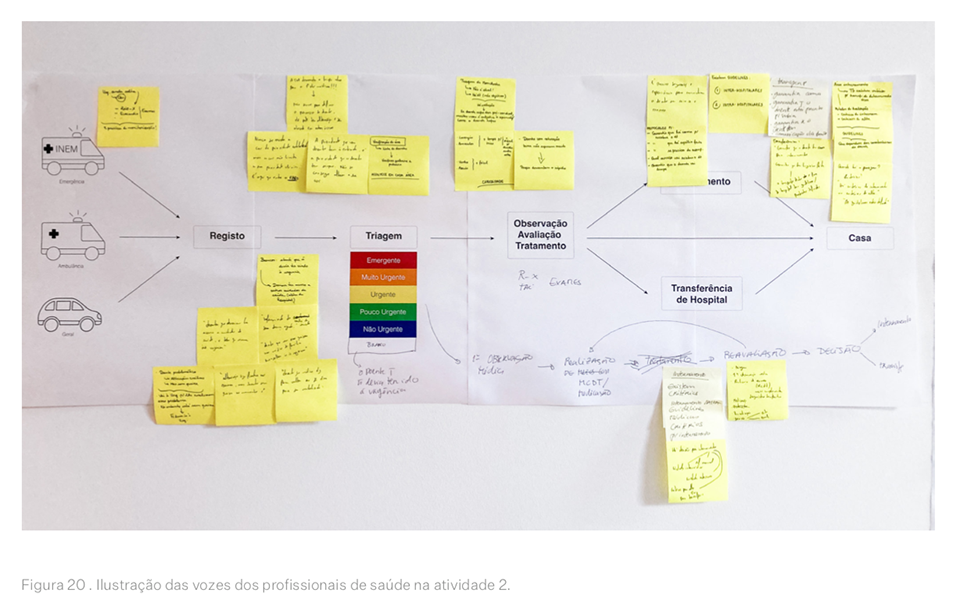
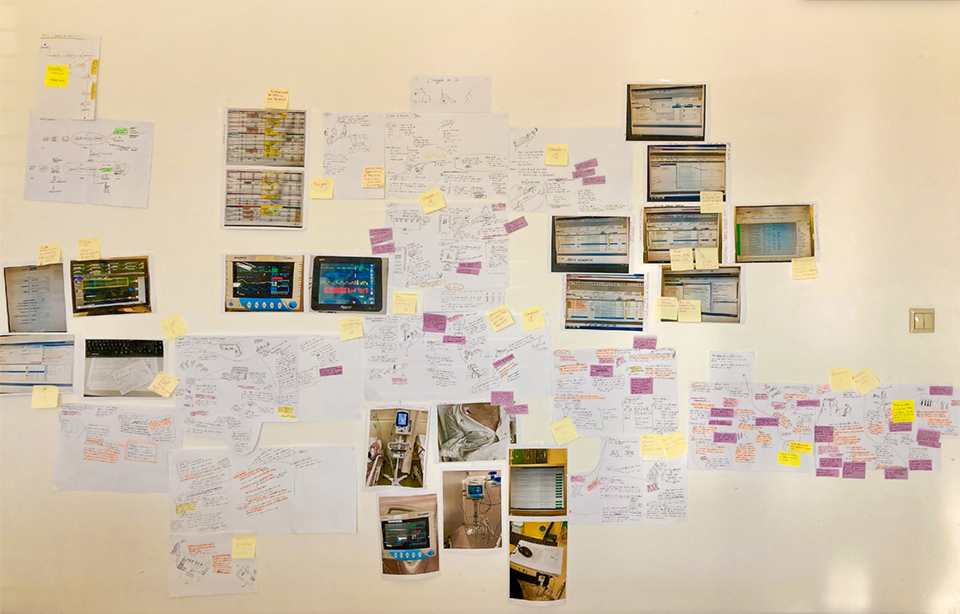
The deterioration of a patient’s health in a hospital emergency department is not always properly recognized, resulting in unplanned admissions, morbidity risks, and unexpected in-hospital deaths. In addition, approximately 31% of patients who appear to be stable, i.e., without a level of urgency, admitted to SUH show signs of deterioration in the following 24 hours. This situation raises concerns about quality of care and its impact on clinical effectiveness, promotion of safety, and user experience. In the last 10 years, efforts have been made in design research to develop a collaborative model to involve health professionals and users directly and actively in the development of health interventions (Neves et al., 2021). In Portugal, recent health quality evaluation reports have identified the need to involve users in the development of health interventions as a priority to ensure improvement in the quality of health care (OECD, 2015). However, it is unclear whether the development of health interventions in Portugal is using a collaborative model and/or using design as an approach or method to do so. This project report reports on the work of the design team in the SafeTrack multidisciplinary project (Portugal Project, 2020), which aimed to use a methodological approach in participatory codesign. It involved the direct participation of health professionals and users to rethink the monitoring of users in hospital emergency services: this project involved four health professionals (three nurses and one doctor) and four representatives of users who had recently been discharged from hospital emergency services. The project was developed in three phases to gather a range of information.
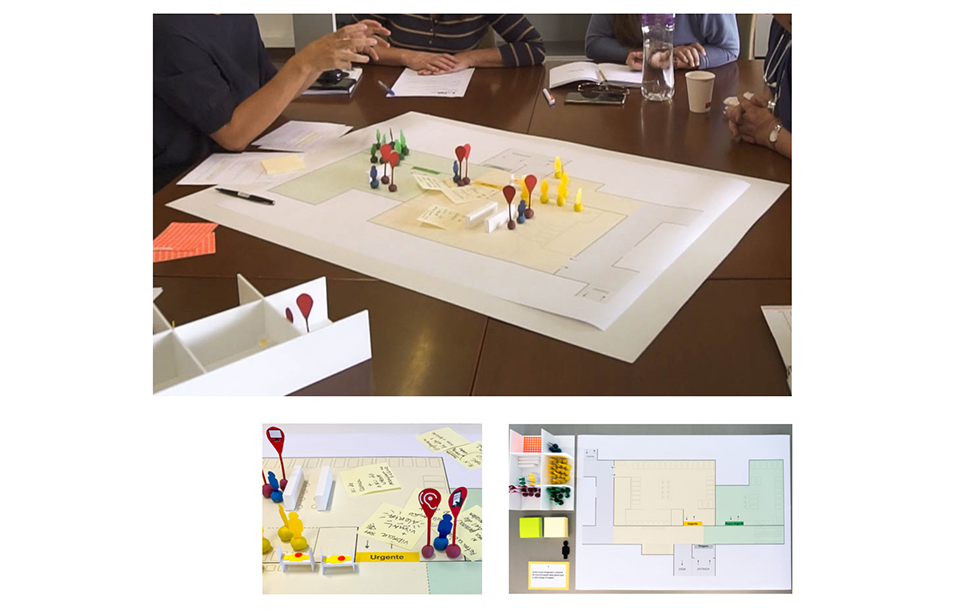
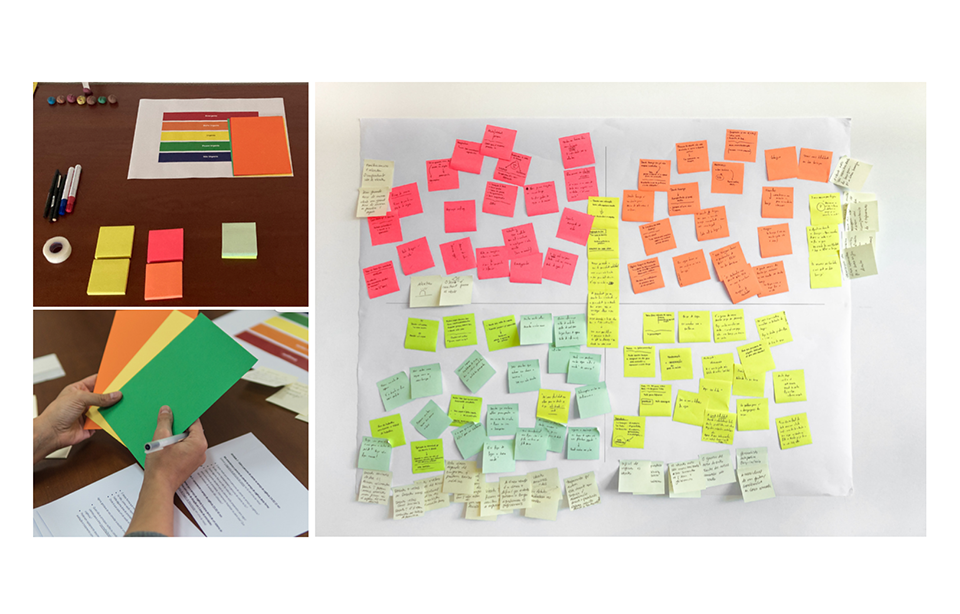
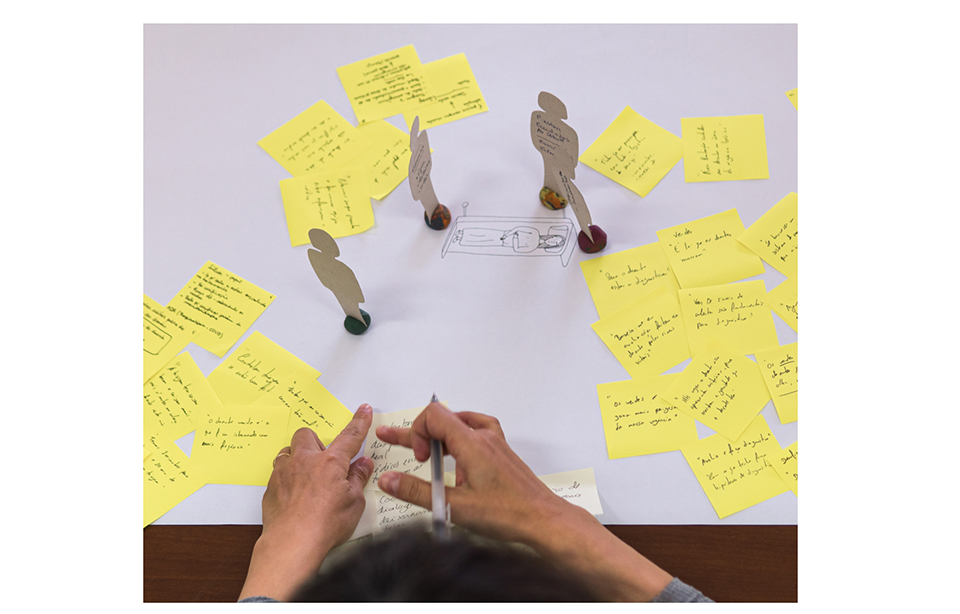
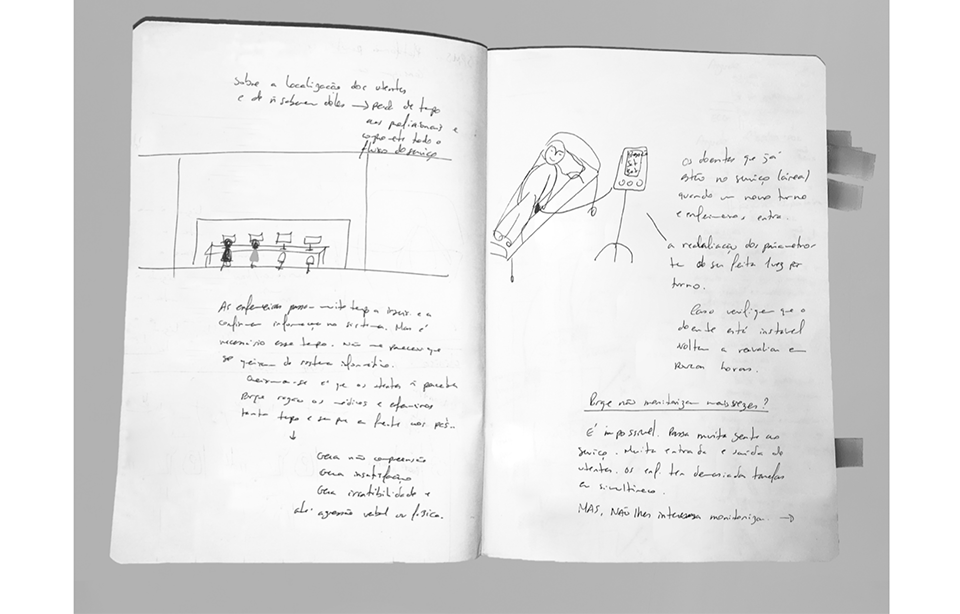
The first phase included observations and two participatory design workshops, the second phase included a co-design workshop, and the third phase initiated the initial prototyping steps, which included individual discussions with designers, engineers, and nurses. The results of the design study demonstrate an understanding of the current state of user monitoring through the diverse perspectives of healthcare professionals and users. The perspectives highlight the need for an integrated patient monitoring system that facilitates the management, coordination, and communication of individual patient information during monitoring.
An understanding of the opportunities for desirable future user monitoring for the SUH is also highlighted. Here, the views highlight the relevance of monitoring as an
early warning system to detect clinical deterioration in the SUH is emphasized. These findings formed the basis for initiating exploratory and prototype developments of
the idealized future patient monitoring system in SUH. In this study, a participatory codesign framework (Neves, 2014) was tested in this SUH context, and was found to be flexible and also beneficial to design research practices in Portugal. It allows for the direct involvement of key stakeholders in the health intervention development process, allows for the exploration of techniques and tools to support the communication of a variety of information based on the sharing of individual experiences and ideas, and provides opportunities to contribute to the decision-making process in this context of user monitoring in the SUH. Therefore, the approach and techniques used in this study can be appropriate for use in other health care settings. This study may also be of interest to other health care communities seeking new ways to improve health care.